Iron Drip
IRON DRIP
Essential Iron
Iron is a vital nutrient that supports overall health and wellbeing. While it is usually obtained through diet, iron plays a crucial role in maintaining both mental clarity and physical performance, as well as sustaining healthy energy levels.
Iron is a key component of haemoglobin, a protein found in red blood cells. Haemoglobin is responsible for transporting oxygen from the lungs to tissues throughout the body. Adequate iron levels help support focus, stamina, and a healthy immune system.
Blood Tests
We ask that you have a Full Blood Count (FBC) and iron studies (including ferritin) completed in advance of your appointment, and that the results are sent to us and available for review before any IV iron treatment is booked or administered. The blood tests must be current, meaning they should have been performed within the last 6 weeks.
It is also helpful, though not essential, to have additional tests including thyroid function, liver function, electrolytes, vitamin D, vitamin B12, and folate (ideally within the last 6 months).
If you do not already have suitable results, testing can be arranged via Medichecks. We can either arrange the full blood test for you or organise a blood draw only if you are arranging the test independently. When arranged through us, results are sent directly to our system, ensuring they are reviewed by our clinical team before your IV iron appointment.
BOOK YOUR CONSULTATION TODAY AND LET'S BOOST YOUR BEAUTY IN EVERY POSSIBLE WAY!
PRICING:
Telephone consultation and bloods review: £50
100mg Iron Sucrose: £175 (most patients require several treatments)
500mg Ferinject: £390 (one treatment is sufficient for most people)
This procedure should only be performed by an experienced Healthcare Professional.
Iron deficiency occurs when the body does not have enough iron to meet its needs. It is the most common nutrient deficiency worldwide.
Iron deficiency can develop gradually and may be present before anaemia is diagnosed. As iron stores become depleted over time, the body produces fewer healthy red blood cells, which can eventually lead to iron deficiency anaemia (IDA).
Symptoms of iron deficiency vary but commonly include persistent fatigue or exhaustion. Low iron levels can affect both mental and physical health. Mental symptoms may include brain fog, difficulty concentrating, anxiety, or low mood. Physical symptoms can include palpitations, shortness of breath or air hunger, chest discomfort, headaches, itching, easy bruising, and in more severe cases, restless legs or pica (such as craving or eating ice).
If left untreated, iron deficiency can have long-term health consequences. Ongoing fatigue and associated symptoms may significantly impact quality of life, reducing daily functioning, focus, and productivity at work and home.
Iron drips are suitable for both women and men. At East Park Healthcare we provide a detailed review to ensure the underlying cause is investigated and managed with a clear treatment plan for patients that includes diet, options for tablets and iron infusions.
For many women the common causes are heavy period or childbirth. An iron infusion is very effective to rapidly correct iron deficiency and anaemia with proven benefits include, vitality, increase quality of life, benefit hair growth, libido, and also improved exercise ability.
Intravenous iron is also beneficial in many illnesses associated with iron deficiency and anaemia, such as; gastrointestinal disease, heart disease, cancer therapy and patients undergoing operations.
Iron is an essential nutrient that helps deliver oxygen and produce energy throughout the body. It is a key component of haemoglobin, the protein in red blood cells that transports oxygen from the lungs to tissues. Iron is also required for enzymes that generate energy in muscles.
When iron levels are low, symptoms may include persistent tiredness and exhaustion, along with a wide range of physical and mental effects.
Physical symptoms can include shortness of breath or “air hunger,” dizziness when climbing stairs, palpitations, chest discomfort, headaches, and in more severe cases restless legs, itching, bruising, and increased hair shedding or breakage.
Mental symptoms may include brain fog, forgetfulness, difficulty thinking clearly or coping, and reduced libido. These symptoms can sometimes be mistaken for anxiety or depression when the underlying issue is iron deficiency.
Adequate iron is essential for producing healthy red blood cells, supporting muscle function, energy levels, brain health, immunity, and overall metabolic processes.
Iron deficiency is diagnosed through blood tests that show low iron levels in the body. Assessment is based on an iron profile, with particular focus on two key markers: ferritin and transferrin saturation.
Ferritin is a protein that stores iron, mainly in the liver. It reflects the body’s iron reserves, and a low ferritin level indicates depleted iron stores.
Iron deficiency is typically defined as ferritin below 30.
Transferrin is a protein that transports iron from storage sites to the bone marrow, where it is used to produce red blood cells. In iron deficiency, transferrin carries less iron, resulting in a low transferrin saturation (“T sats”).
Diagnosis and thresholds are in line with NICE clinical guidance on iron deficiency anaemia.
https://cks.nice.org.uk/topics/anaemia-iron-deficiency/
Iron is essential for the production of haemoglobin and healthy red blood cells, which transport oxygen around the body. Iron acts as a key building block for red blood cells. When iron levels are low, the body produces less haemoglobin and fewer red blood cells.
As red blood cell production decreases, the number of circulating red cells falls, leading to anaemia. Anaemia is defined by a low haemoglobin level in the blood:
Women: Hb < 120 g/L
Men: Hb < 130 g/L
Even before anaemia develops, iron deficiency affects red blood cell quality. The cells produced are often smaller than normal (microcytic, reflected by a low MCV) and contain less haemoglobin (low MCH). For this reason, maintaining adequate iron levels is essential for healthy oxygen delivery and overall wellbeing.
Most iron in the body is found in red blood cells and muscles. In total, the average adult has around 4,000 mg of iron, with approximately 2,500 mg used to form haemoglobin, the protein in red blood cells that carries oxygen.
As red blood cells age, they are broken down in the spleen and the iron is efficiently recycled. Although a small amount of iron is lost each day through skin shedding and sweat (around 2–3 mg daily), this is normally replaced through the diet, helping maintain healthy iron stores.
Iron is transported around the body by a protein called transferrin and stored mainly as ferritin, the body’s iron reserve. Around 1,000 mg of iron is held in ferritin stores, while the remaining 500 mg is used by cells—particularly muscles and nerves. Within cells, iron is essential for enzymes involved in aerobic metabolism, allowing the body to produce energy from oxygen and food.
Iron deficiency can develop for several reasons, most commonly due to reduced intake, poor absorption, or increased iron loss.
Dietary factors
Not consuming enough iron-rich foods is a common cause. Meat is the most efficient source, with around 10–20% of iron being absorbed, compared to only 1–2% from plant-based sources. This means people following vegetarian or vegan diets are at higher risk. Other iron-rich foods include fortified cereals, soya, and pulses such as lentils. Around 2–4 mg of iron needs to be absorbed daily. Iron absorption is reduced by low stomach acid, antacid medications (such as omeprazole), and drinking tea close to meals, while vitamin C can enhance absorption. Simple dietary changes can therefore make a meaningful difference.
Blood loss
In women, the most common cause is menstrual blood loss. Even “normal” periods can result in the loss of up to 40 mg of iron per month. Heavy menstrual bleeding (HMB) is very common, affecting around one in three women at some point, and can lead to significant iron depletion over time.
Pregnancy and childbirth
Pregnancy places high iron demands on the mother, with the developing baby requiring large amounts of iron. Blood loss during delivery, particularly with caesarean section, can further reduce iron levels.
Reduced absorption and chronic conditions
Conditions that affect the gut, such as coeliac disease or inflammatory bowel disease (including Crohn’s disease and ulcerative colitis), can impair iron absorption. Chronic inflammation and long-term conditions such as arthritis or diabetes may also contribute.
Surgery
Iron deficiency can occur after surgery due to blood loss, or following bariatric (weight loss) surgery where parts of the intestine responsible for iron absorption are bypassed.
Treatment depends on the severity of iron deficiency, symptoms, and how well iron is absorbed. Options range from dietary changes and oral supplements to intravenous iron therapy.
Diet and oral iron supplements
A balanced diet that includes iron-rich foods such as meat, pulses, and soya is important. For many people with mild iron deficiency and minimal symptoms, oral iron tablets are an effective first-line treatment.
Most iron tablets contain iron salts, such as sulphate, gluconate, fumarate, or bisglycinate. While tablets may be labelled as 200–300 mg, the key factor is the amount of elemental iron they contain (often around 60–70 mg per tablet). This is the actual dose your body can use.
Iron absorption from the gut is limited, with only around 4–6 mg absorbed per day. Several factors can improve absorption:
Taking iron on an empty stomach, ideally in the morning
Having an acidic stomach environment
Avoiding proton pump inhibitors (PPIs) such as omeprazole
Avoiding tea or coffee around the time of dosing
Taking iron with vitamin C
Avoiding multivitamins at the same time, as they can interfere with absorption
Dosing and duration
One iron tablet (200–300 mg) per day is usually sufficient. If side effects such as abdominal discomfort, constipation, or diarrhoea occur, stopping for five days and restarting on alternate days often improves tolerance.
Most people begin to see improvement in haemoglobin levels within 4–6 weeks, but iron supplements usually need to be continued for 3–9 months to fully restore iron stores.
Monitoring and targets
Blood tests should be repeated 2–3 months after starting treatment to check haemoglobin (Hb) and ferritin levels. Iron tablets should be stopped for 3–5 days before testing to ensure accurate results. Treatment is usually continued until ferritin is above 50.
When to consider iron infusion
If, after around three months of oral iron therapy, ferritin levels have not improved towards 30, this suggests poor absorption or intolerance to tablets. In this situation, an intravenous iron infusion should be considered.
Modern iron infusions use advanced formulations developed over the past decade, allowing a full replacement dose of iron to be given safely in as little as 30–60 minutes. This makes it possible to deliver the amount of iron needed to restore normal iron stores in a single treatment.
An iron infusion is significantly faster and more effective than oral iron tablets, particularly for people with moderate to severe deficiency or poor absorption. Typical prescribed doses range from 500 mg to 1,500 mg, providing a “total dose” that rapidly replenishes iron levels.
Because the iron is delivered directly into the bloodstream, it is immediately available to the bone marrow and muscles where it is needed to produce healthy red blood cells and support energy levels. Many people notice improvement in symptoms within days, and as iron stores are restored in one treatment, further tablets or repeat treatments may not be required.
Overall, iron infusions are considered very safe and are comparable in risk to receiving an intravenous antibiotic. Many people feel reassured after an initial consultation, which allows time to review information, ask questions, and understand exactly what to expect before treatment.
Before your appointment
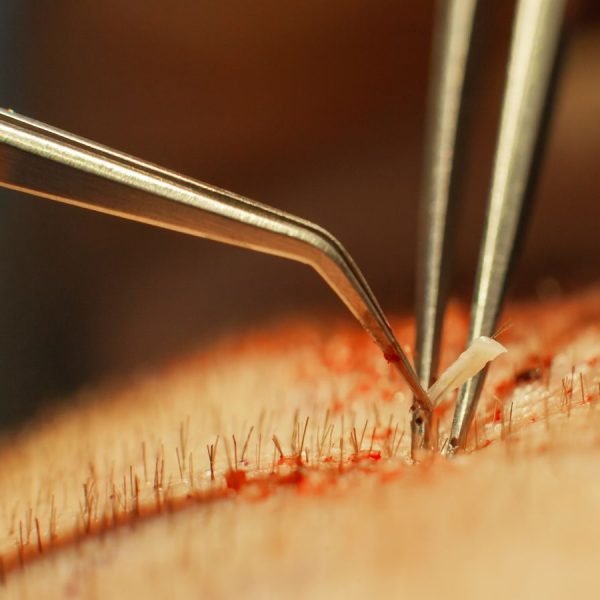
We recommend eating a normal breakfast and lunch and ensuring you are well hydrated. Good hydration helps with placing the drip (cannula) safely into a vein. Before the infusion starts, the cannula is carefully checked with a saline flush to ensure it is correctly positioned. Very rarely, iron can leak into surrounding tissue, which may cause a brown skin stain. While this is uncommon, it can be permanent, which is why extra care is taken with cannula placement, including additional flushing or using a saline drip beforehand. On rare occasions, the cannula may need to be repositioned or the infusion rescheduled to minimise this risk.
Common side effects
Most people tolerate iron infusions very well. Pre-medication is not routinely used, as it can sometimes cause side effects itself.
A short-lived flushing reaction (known as a Fishbane reaction) occurs in around 1–2 in 100 people. This may include flushing, light-headedness, nausea, chest tightness, dry cough, or dizziness. This is not an allergy but a temporary reaction of the blood vessels to iron, similar to the flushing some people experience with CT or MRI contrast. For safety, infusions are started slowly and you are closely monitored. If symptoms occur, the infusion is stopped and symptoms usually settle within seconds. Treatment can then be restarted slowly if appropriate.
Skin reactions
Hives or a rash can occur in approximately 1 in 200–500 people, which is why we ask patients to remain in the clinic for 30 minutes after treatment. These reactions usually respond well to antihistamines. If you have a history of allergies or hives, taking an antihistamine beforehand may be advised.
Rare and serious reactions
More severe reactions are uncommon. Swelling of the hands or feet can occur, and very rarely, allergy-type reactions such as difficulty breathing, chest tightness, dizziness, itching, or swelling of the lips may develop. The clinical team is fully trained to manage these events, with appropriate equipment and protocols in place.
Overall, around 3% of people experience any side effects from intravenous iron, the vast majority of which are mild and short-lived. Serious reactions are extremely rare, occurring in fewer than 10 per million treatments. Large reviews, such as(JAMA 2016), have shown that modern IV iron preparations carry a similar risk to many commonly used infusions and are significantly safer than blood transfusion .
Once your infusion has finished, we will check that you are feeling well, repeat your observations, and remove the cannula. You will then be asked to remain in the clinic for 30 minutes for observation. If you notice any symptoms such as a rash or hives during this time, please inform a member of the team. After this observation period, you will be free to go home.
Post-infusion symptoms
Around 1 in 4 people experience what is commonly known as a post-infusion flu. This usually starts about 24 hours after treatment and may feel like a flu-type illness, with muscle or joint aches, tiredness, feeling unwell, and occasionally a mild temperature. This reaction is thought to be a type of “serum sickness.” It is usually short-lived, settling within 24–48 hours, though in some cases it may last up to a week. Staying well hydrated and using standard over-the-counter pain relief can help manage symptoms.
Phosphate levels after infusion
With certain iron preparations, particularly ferric carboxymaltose (Ferinject), a temporary drop in blood phosphate levels can occur 2–3 weeks after infusion. This happens in up to half of patients receiving this formulation, although it is usually mild and does not cause symptoms. Studies have shown no clear link between phosphate levels and post-infusion symptoms in otherwise healthy individuals.
In rare cases, mainly in people requiring frequent, repeated infusions, low phosphate levels have been associated with bone health concerns. For this reason, we avoid repeat dosing with Ferinject and use alternative preparations, such as Monofer, in patients needing long-term treatment. Only a very small number of cases have been reported across the wider clinical setting, with symptoms most commonly described as fatigue or a general feeling of being drained.
There are currently no clear risk factors for hypophosphataemia in healthy individuals, and routine phosphate testing or supplementation is not recommended. In most cases, levels return to normal on their own over time. Vitamin D may be helpful and is unlikely to cause harm, but specific treatment is rarely required. Any concerns should always be discussed with your clinician.
Putting risk into perspective
Our Clinical team continually review and update our guidance in line with the latest evidence. More than 60 million IV iron infusions have been given worldwide in the past decade, and for many people this treatment is truly life-changing. While no medical treatment is completely risk-free, every effort is made to minimise risks and ensure treatment is delivered safely and appropriately.